Welcome To Our Blog!
Welcome to the Cary Eye Center Blog. stay Tuned for new posts and the latest news!
The normal retina is shown in Fig. 1. The round optic disc is seen with normal appearing blood vessels coming out and a normal retina and macula (the center part of the retina that corresponds to our clearest, central vision). The retinal veins are darker and larger than the retinal arteries.
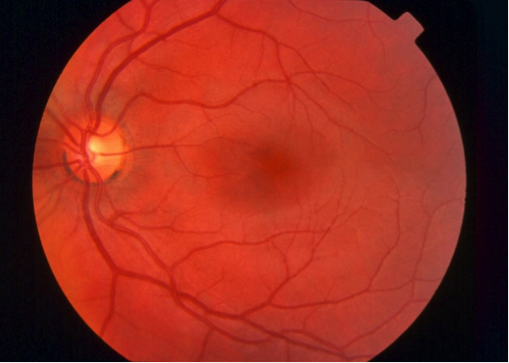
Figure 1
In Fig. 2, we can see some of the early signs of Diabetic Retinopathy. The scattered red spots are called dot and blot hemorrhages and there are some tiny spots that are called microaneurysms. The blood vessels also begin to become abnormal, in this case the white rectangle is showing “venous beading”. Also, some of the small white spots represents exudates and the larger white areas correlated to damage of the nerve fiber layer, called cotton wool spots. Each of these findings correlates to the first stage of Diabetic Retinopathy, called Non-Proliferative Diabetic Retinopathy, or NPDR.
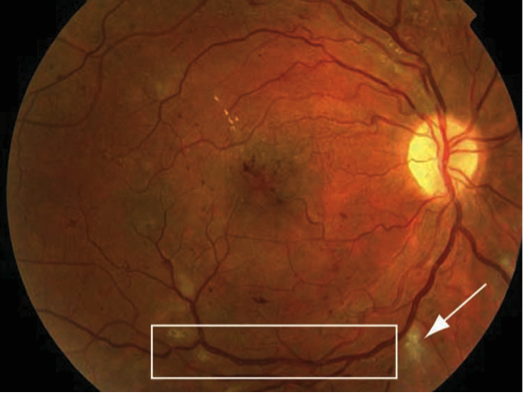
Figure 2
As diabetic retinopathy progresses, it changes from Non-Proliferative to Proliferative Diabetic Retinopathy, or PDR. In Fig. 3, we can see the changes associated with this condition. New, abnormal blood vessels actually begin to form, a process called neovascularization (NV). These can occur near the optic disc (NVD) or in other parts of the retina (elsewhere), termed NVE. In Fig. 4A, some of these acronyms are noted in the diagram. PDR is a very serious condition and can cause hemorrhaging, retinal swelling, scar tissue formation, and retinal detachment. In addition to the aforementioned blood sugar control, laser treatment must be initiated for PDR, as well as sometimes for severe NPDR. The laser treatment is applied to the peripheral retina in little spots, as shown in Fig. 4B. This treatment, while not a cure, can help reduce the ischemic load of PDR and slow down its progression. It will also help to prevent another complication of PDR which is called neovascular glaucoma.
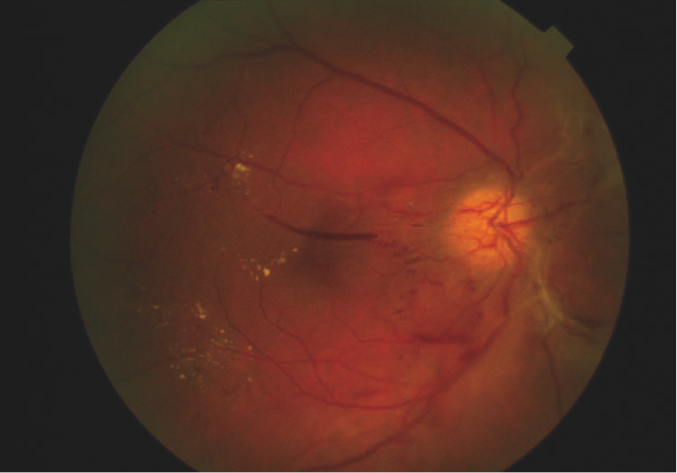
Figure 3
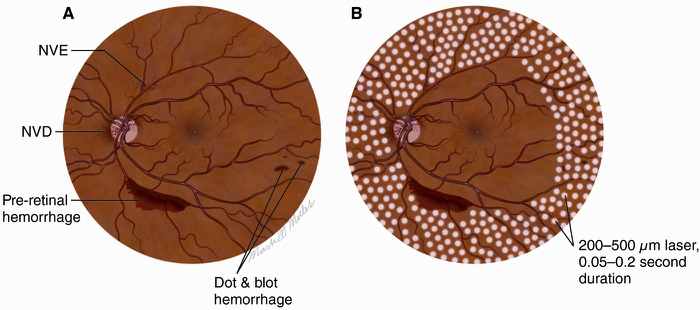
Figure 4
PDR often results is severe hemorrhage that can move out of the retina and into the center part of the eye, called the vitreous. When this happens, it is termed a Vitreous Hemorrhage (VH) (Fig. 5). The dark red spots are the VH. If severe enough, the VH can fill the entire eye, making the person effectively blind. This blood can usually, however, be removed with a surgical procedure.
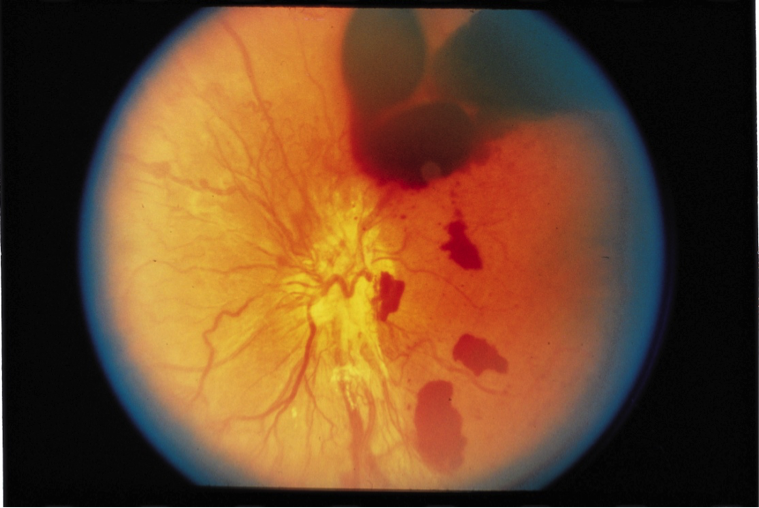
Figure 5
A final visual problem associated with Diabetic Retinopathy is swelling in the center part of the retina, the macula, where our central vision is located. This is termed Diabetic Macular Edema (DME). The retina is normally flat, akin to a dry sponge. Due to leakage of fluid, diabetics can experience swelling in the macula, which causes blurry vision. A diagram of this condition is shown in Fig. 6. The top part of this figure shows a diagram of the anatomy of the macular in DME (Fig. 6A). Below it, there is a real OCT image of a swollen macula with DME (Fig. 6B). OCT, which stands for Ocular Coherence Tomography, is a relatively new technology that takes a “slice” of the retina to determine the health of this detailed anatomy. The large black cystic spaces are representative of fluid accumulation, like a wet sponge. Below this image is an OCT of a normal macula (Fig. 7) for comparison.

Figure 6
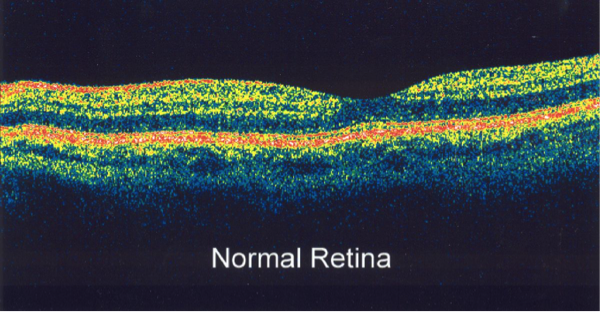
Figure 7
Figures 1-7 are © 2015, American Academy of Ophthalmology.